Context : The National Centre for Disease Control (NCDC) has officially refuted the findings of a recent international study published in The Lancet’s eClinicalMedicine claim that over 50% of Indian patients undergoing a specific gastrointestinal procedure were colonised with Multi-Drug Resistant Organisms (MDROs), terming it a “global threat.”
Fundamentals of Antibiotics & Drug Resistance
- Definition: Biological agents designed to neutralize bacteria within the body without harming the host. They are critical for surgeries, chemotherapy, and treating bacterial infections.
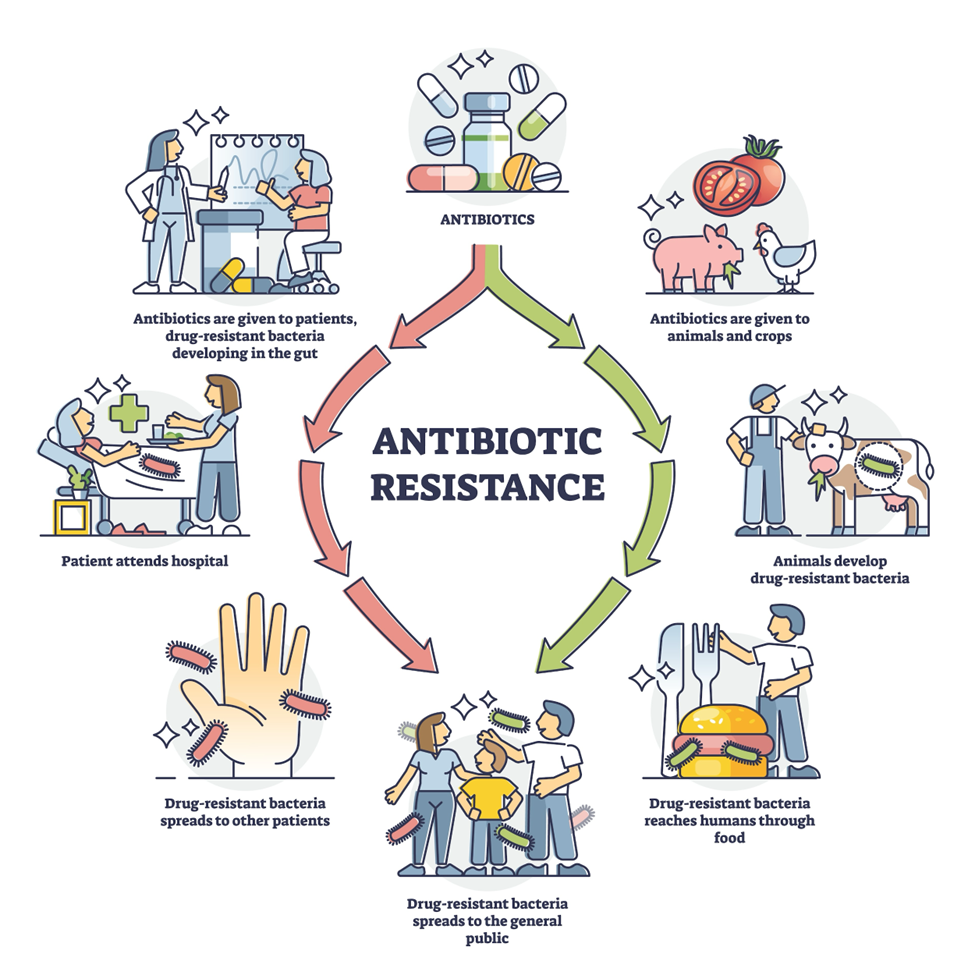
- Mechanism of Resistance: When antibiotics are overused, bacteria adapt and evolve to survive the drug’s effects. This renders the drug ineffective over time, leading to “Drug Resistance.”
- Impact: Resistance complicates treatment, necessitates stronger/more expensive drugs, prolongs illness, and increases mortality rates (e.g., Multidrug-resistant Tuberculosis).
Understanding Antimicrobial Resistance (AMR)
- Scope: AMR is a broader term encompassing resistance in all microbes (bacteria, viruses, fungi, parasites), whereas antibiotic resistance is a specific subset limited to bacteria.
- Transmission: Resistant microbes are found in humans, animals, and the environment (soil, water). They spread via person-to-person contact, food of animal origin, and environmental contamination.
- Global Threat: The UN places the threat of AMR on par with Ebola and HIV. The WHO identifies it as one of the top ten threats to global health.
Primary Drivers of Resistance
- Inappropriate Usage: The consumption of antibiotics for viral infections (like the common cold or flu) where they are ineffective.
- Zoonotic Transfer: The rampant use of antibiotics in livestock and poultry for growth promotion. These residues enter the human body through the food chain.
- Environmental Contamination: Improper disposal of residual antibiotics and inadequately treated sewage introduce resistant bacteria into the ecosystem.
- India’s Landscape & Policy Framework
- Status: India is the world’s largest consumer of antibiotics, leading to rapid bacterial mutations.
National Policy for Containment of AMR (2011):
- Objective: To understand the emergence of AMR and rationalize the use of antimicrobials.
- Key Action Points:
- Establishment of a robust AMR surveillance system.
- Strengthening infection prevention and control measures.
- Regulating the private health sector and strictly monitoring drug sales.
- Educating stakeholders on the prudent use of drugs.
Global Initiatives & WHO Guidelines
- Surveillance: Launch of the Global Antimicrobial Surveillance System (GLASS) in 2015 to standardize data collection across countries.
Recommendations:
- Prioritize National Action Plans with scaled-up financing.
- Invest in R&D for new technologies and drugs.
- Enforce stronger regulatory systems for drug distribution in human and animal health sectors.