Why in the News?
A recent article highlights the gaps in India’s mental-health ecosystem and argues that mental health care must be re-imagined through the lens of disability justice, dignity, inclusion and relational support, rather than narrow clinical or biomedical interpretations.
Background: Distress Beyond Diagnostics
- Survivors of childhood abuse, neglect, trauma and deprivation often describe lifelong emotional wounds that are not captured by numeric clinical scales or diagnostic manuals.
- Dominant narratives pathologise people as “unmanageable”, ignoring structural factors such as poverty, violence, social barriers, stigma and inadequate care systems.
- The current mental-health system continues to adopt individualised, clinical, symptom-focused frameworks where:
- Medicines promise fewer side-effects but do not answer fundamental questions.
- Lived experiences are interpreted through productivity-centric and medicalised lenses.
- Social and contextual dimensions remain overlooked.
The Gaps in Current Mental-Health Care
a) Over-medicalisation and narrow definitions
- Biomedical models dominate diagnosis and treatment.
- Distress is labelled “maladaptive” or “pathological”, ignoring histories of trauma, economic precarity and social marginalisation.
b) Fragmented approach
- Emotional, social, cognitive and physical determinants of distress are treated in silos, not holistically.
- National Crime Records Bureau (NCRB) data shows suicides are high among daily-wage earners, indicating systemic vulnerabilities, not individual weakness.
c) Lack of continuity, trust, and community
- People disengage from services due to broken trust, impersonal responses, stigma, and lack of long-term support.
- Mental-health outcomes deteriorate when people feel unheard or excluded.
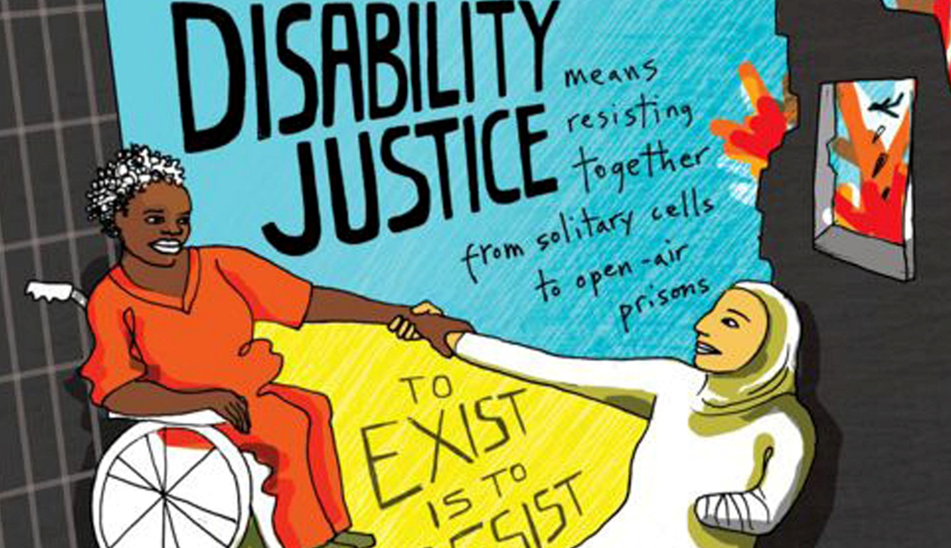
Need for a Paradigm Shift: Mental Health as Disability Justice
a) Re-imagining care
The article argues that mental health must be placed within a disability justice framework that centres:
- Dignity, inclusion and agency
- Relational support (family, community, social connections)
- Lived experiences over mere clinical metrics
This moves focus from “fixing an individual” to understanding conditions that shape suffering.
b) Recognising multiple determinants
Distress often stems from:
- Trauma (interpersonal, historical, institutional)
- Economic precarity
- Caste and gender violence
- Neoliberal expectations of productivity
- Social isolation
- Cultural norms, stigma, and exclusion
Hence, care must address intersecting social oppressions, not just symptoms.
What Justice-Oriented Mental Health Care Should Look Like
a) Shifting emphasis from cure to connection
- Care should cultivate solidarity, safety, relationships, and belonging.
- Community-based supports, peer networks and non-linear healing pathways should be valued.
- Focus on life that feels liveable, not merely symptom reduction.
b) Beyond redistribution to recognition
- Justice means not only providing services and resources but also recognising different worldviews, moral frameworks and relational ecosystems.
- This involves:
- Listening to lived experiences
- Acknowledging structural harm
- Adapting care to diverse identities and contexts
c) Transforming systems – education, practice & research
Future mental-health practice must:
- Capture granular, experiential aspects of distress
- Work with uncertainty rather than forcing neat categories
- Integrate social sciences, disability studies and qualitative research
- Reject one-size-fits-all solutions
- Build long-term collaborations, trust, and continuity
This represents a shift from diagnose-treat-discharge to long-term, dialogic, inclusive engagement.
Way Forward
1. Strengthen community-based care
- Implement the District Mental Health Programme (DMHP) using peer-support systems and community workers.
2. Training health professionals
- Include psychosocial disability frameworks, trauma-informed care and cultural competency in curricula.
3. Expand social security and economic safety nets
- Reduce distress stemming from poverty, debt, unemployment and precarious livelihoods.
4. Legal & policy alignment
- Integrate the Mental Healthcare Act (2017) with the Rights of Persons with Disabilities Act (2016) to ensure:
- Dignity
- Non-discrimination
- Supported decision-making
5. Promote lived-experience leadership
- Involve people with psychosocial disabilities in policy design, service delivery and evaluation.
Conclusion
Mental health care in India needs radical transformation. A disability justice-oriented approach demands that care:
- centres dignity, trust and inclusion,
- recognises social and structural roots of distress, and
- values diverse experiences beyond clinical labels.
Only then can the system shift from treating illness to fostering wholeness and well-being.
Source: Care as disability justice, dignity in mental health – The Hindu
UPSC CSE PYQ
| Year | Question |
| 2024 | Mental healthcare remains one of the most neglected areas of public health in India. Discuss the challenges and suggest reforms. |
| 2023 | Discuss how poverty, social exclusion and inequality worsen the mental health crisis in India. |
| 2023 | Highlight the role of social institutions in shaping mental and emotional well-being in contemporary society. |
| 2022 | The Mental Healthcare Act, 2017 marks a shift from a medical model to a rights-based approach. Examine. |
| 2022 | Analyse how trauma and social oppression affect psychological well-being and social behaviour. |
| 2021 | Discuss the issues faced by persons with disabilities in accessing health and education services in India. |
| 2020 | How do empathy and compassion improve the quality of care in public service delivery, especially in mental health? |
| 2019 | Discuss the challenges in implementing community-based mental-health programmes in India. |
| 2019 | What are the psychological and social impacts of childhood trauma on adult behaviour? |
| 2017 | Discuss the importance of rights-based frameworks for persons with disabilities. How far has India progressed? |
| 2015 | Discuss ethical challenges faced by caregivers and health workers while supporting mentally vulnerable individuals. |
| 2014 | Assess the challenges faced by disabled people in securing dignity, rights and social inclusion in India. |
| 2013 | Discuss the status of mental-health infrastructure in India and the need for community-based approaches. |
| 2013 | How do social, cultural and economic factors shape mental-health vulnerabilities in India? |